While the race to find a vaccine to the coronavirus is picking up momentum as we speak, let’s not forget about the medicines and vaccines that are already in use, or are in the process of being tested for use. T cells and dendritic cells are some of the most important components of an individual’s immune system. A T cell is a kind of white blood cell that is often found in the thymus because its maturation takes place there. A dendritic cell is considered one of the best antigen-presenting cells and has the ability to activate naive T cells. It consists of pattern recognition receptors that can detect components of foreign microbes. Therapies that take advantage of the mechanisms of T cells and dendritic cells are currently in development. Some have even become established therapies that are used commonly today.
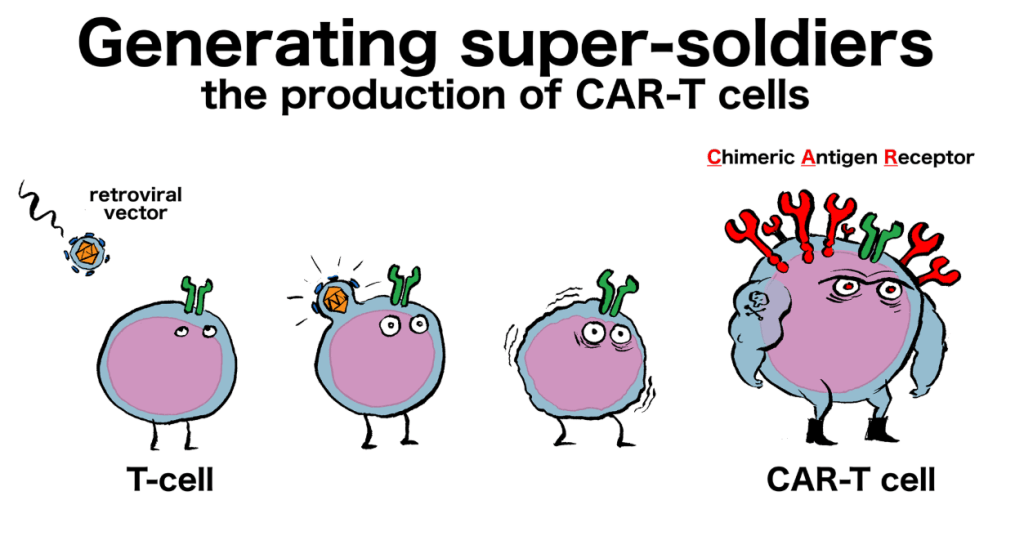
According to an article from Genetic Engineering and Biotechnology News, researchers from Baylor College of Medicine have reported their findings on an improved CAR T cell therapy commonly used to treat people with acute lymphoblastic leukemia (ALL). Acute lymphoblastic leukemia is a kind of cancer that primarily occurs in children and concerns white blood cells found in bone marrow and blood. It is an acute disease because it has a fast progression and can be detrimental. This therapy is often used alongside chemotherapy because chemotherapy may not be enough to combat this disease. CAR T cells, specifically those that consist of three prongs, are much more effective fighting against this cancer than those that only consist of one or two prongs. CAR stands for chimeric antigen receptors. The addition of prong(s) can increase the number of antigens that the modified T cell can recognize. This can lead to an attack on cancer cells found in the body. Moreover, researchers are able to use T cells from affected individuals and alter what proteins they have the ability to target by adding CARs. In this case, instead of only targeting CD-19, the altered T cell can recognize CD-20 and CD-22 as well. These are all located on leukemia cells. They would then reinfuse these cells back in the body so that they can find and target the cancer cells. Before, they only altered the T cell so that it could only target one of these proteins. If there is only one prong, then cancer cells have a higher chance of getting past T cell mechanisms. Since this therapy tinkers with white blood cells, a potential side effect of this therapy could be a decrease in the number of white blood cells in an individual’s body. In addition, this therapy may cost hundreds of thousands of dollars (a good estimate would be $400,000) if this therapy passes its trials.
Prior to reading this article, I was unfamiliar with the idea that people could alter other people’s T cells so that they have the ability to target proteins that only certain types of cells express. I realize now how important it is to be able to tweak any T cell so that it can detect the antigens that it needs to. As we learned in class, if T cells are not able to detect the antigen, they cannot induce mechanisms to kill the infected cell and activate B cells. It is nice to take a break from the COVID-19 news and read about major advances in medicine and treatment concerning other diseases. It gives me hope that there is a possibility that researchers and scientists will find a vaccine or other treatment that will help protect the public from the coronavirus.
In addition, according to an article from Frontiers in Immunology, T cell therapies are currently being investigated in human immunodeficiency virus (HIV) diseases as well. As mentioned in the name, the human immunodeficiency virus is the causative agent of this disease. This virus is known to attack macrophages and helper T cells. If the level of helper T cells gets too low, then the HIV disease may result in acquired immunodeficiency syndrome (AIDS). This research has occurred for a few decades by several people. However, researchers now report that cytotoxic (CD8+) T cells can possibly be modified so that they have a CAR that allows them to target HIV antigen(s). By reintroducing these cells into the body via infusion, the body can better find and fend off this virus so that the virus stops or slows down replication. They believe that this could work because people with a better ability to hold off the replication of HIV had stronger responses from their CD8+ T cells. While HIV-specific CD8+ T cells are still up in the air for HIV disease, it is worth taking a look at. Since it often does not have a prolonged existence after infusion, there may be recurring treatments that add up to hundreds of thousands of dollars (similar to the amount of money for CAR T cell treatment for leukemia). A possible side effect could be neurotoxicity because the dose of CAR T cells could affect the overall inner-workings of the body.
Learning about another way researchers have used or are going to use T cell therapy emphasizes the importance of T cells in how the body functions. I was not aware that it was possible for some people to contain the HIV replication better than others because of how their CD8+ T cells worked. I hope that researchers decide to add additional CARs to individual T cells, if they have not already, because it seems to be showing good results in the tests with trivalent CAR T cells in treating acute lymphoblastic leukemia. This is definitely a difficult subject to grasp in my opinion, but after putting much time and effort into reading and re-reading these articles, I have found a greater appreciation for the current workings of personalized medicine.
As always, stay home and stay safe! ❤
